
High Density Lipoproteins May Actually be Some Negative Acute Phase Proteins in the Plasma
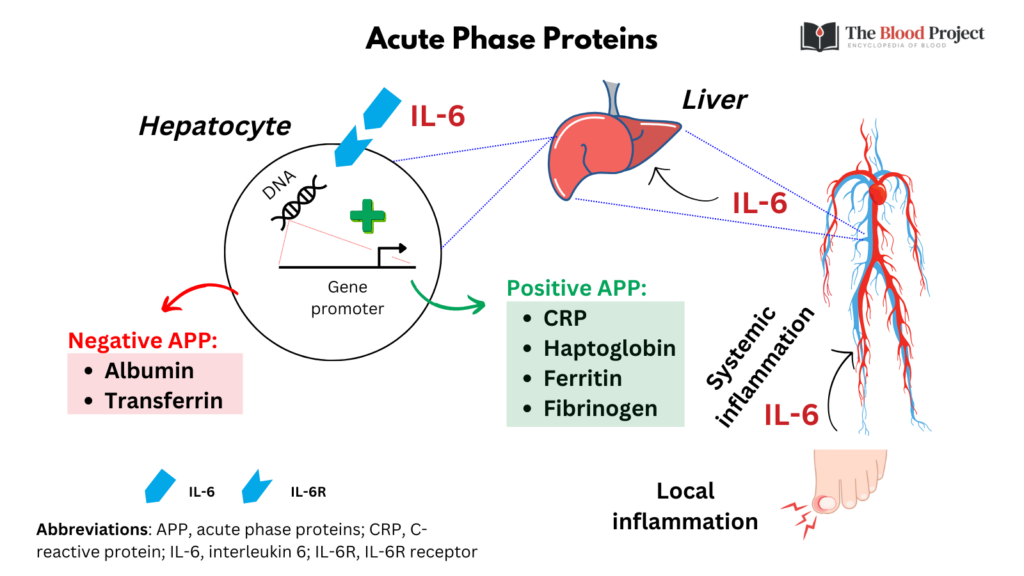
Negative acute-phase proteins. The liver responds by producing a large number of APRs. At the same time, the production of a number of other proteins is reduced; these are therefore referred to as "negative" APPs. Negative APPs are albumin, transferring, transthyretin, transcortin, and retinol-binding protein.

P Proteins Astral Projection
Negative acute phase proteins decrease in plasma concentration by greater than 25% in response to inflammation. This reduction can occur rapidly (within 24 hours) or may decrease gradually over a period of days. The two main negative acute phase proteins are albumin and transferrin. The mechanism by which their concentrations decrease is likely.

Positive & Negative Acute Phase Proteins (Note Those increased during inflammation are
During the acute phase response the demand for amino acids for synthesis of the positive acute phase proteins is markedly increased, which necessitates reprioritization of hepatic protein.
PPT Labs Indicators for Nutritional Intervention PowerPoint Presentation ID6920966
Since transthyretin, a negative acute-phase protein, inhibits interleukin-1 production by monocytes and endothelial cells, 51 a decrease in its plasma concentration may be proinflammatory.

Acute Phase Protein Protein Choices
A systemic acute phase reaction may develop during infection and inflammation, due to the action of peripherally liberated proinflammatory cytokines. Hepatic metabolism changes, and negative and positive acute phase proteins (APPs) can be measured in the blood: the APPs therefore represent appropriate analytes to assess health.

What is the Difference Between Positive and Negative Acute Phase Proteins Compare the
The acute-phase proteins involved in free iron control include the circulating peptide hormone hepcidin, ferritin, haptoglobin, and hemopexin, which are up-regulated in the acute-phase reaction, whereas transferrin is a negative acute-phase protein that is down-regulated during the acute phase (Table 1). Hepcidin binds the transmembrane protein.

Humoral Innate Immunity and AcutePhase Proteins NEJM
During inflammatory disorders, negative acute-phase proteins are downregulated by 25 % (Morley and Kushner 1982) to increase the capacity of the liver to synthesize the induced APRs, e.g., albumin, transferrin, retinol, binding protein, etc. Their reduction indicates a transient increase in free hormones bound to these proteins.

Positive and Negative Acute phase Reactants Mnemonic
The latter proteins have become known as the negative acute phase proteins. An acute phase response can be readily and reproducibly induced in experimental rats by subcutaneous injection of a small amount of mineral turpentine to produce a transient acute inflammation. The simultaneous decrease in the plasma concentration of negative acute.
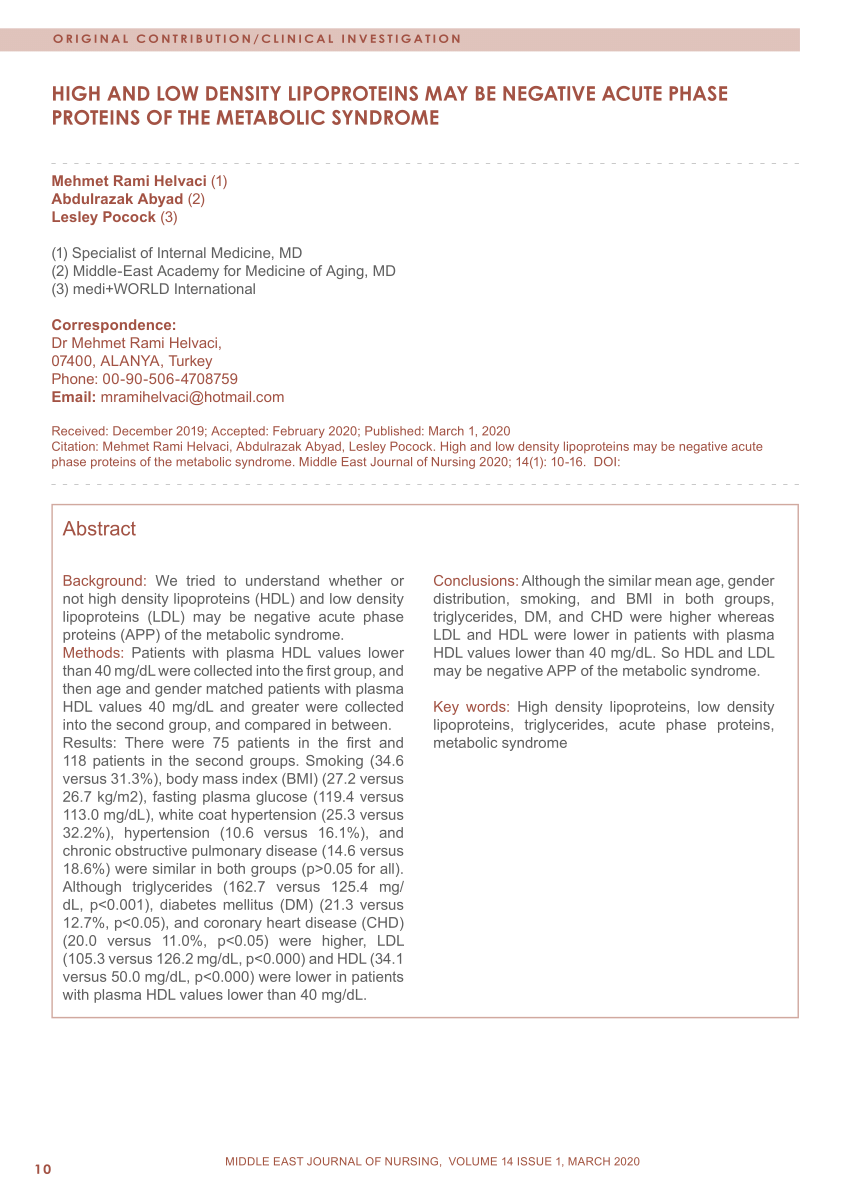
(PDF) High and Low Density Lipoproteins May Be Negative Acute Phase Proteins of the Metabolic
The negative acute phase proteins are therefore described by some authors as 'acute booster reactants' (Ingenbleek and Young, 1994). In malnutrition and chronic infections the response of positive acute phase variables may be less evident (Morlese et al., 1998; Stephensen, 1999).

The constellation of vitamin D, the acutephase response, and inflammation Cleveland Clinic
THE CASE FOR VITAMIN D AS A NEGATIVE ACUTE-PHASE REACTANT. The short answer is yes, there is compelling evidence that 25(OH)D is a negative acute-phase reactant—its serum levels decrease in the presence of inflammatory states. 8-11 Several lines of evidence support this conclusion: Serum C-reactive protein and 25(OH)D levels are inversely associated, as would be expected if 25(OH)D were a.
Acute phase proteins how they are useful for practitioners Vet Times
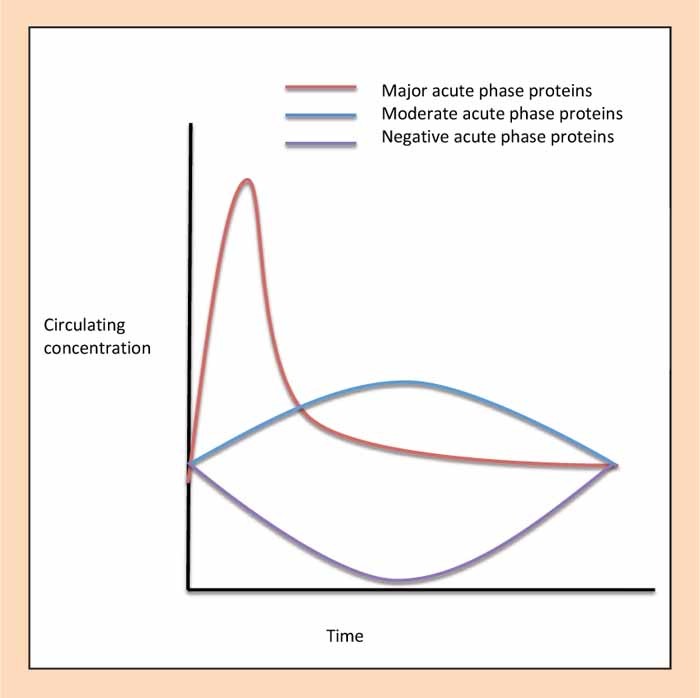
By definition, an acute-phase protein is one whose concentration in the plasma increases (for a 'positive' acute-phase protein) or decreases (for a 'negative' acute-phase protein) by at least 25 per cent during the acute phase (approximately the first 7 days) of inflammatory conditions (Morley and Kushner, 1982; Steel and Whitehead.
Acute Phase Proteins • The Blood Project
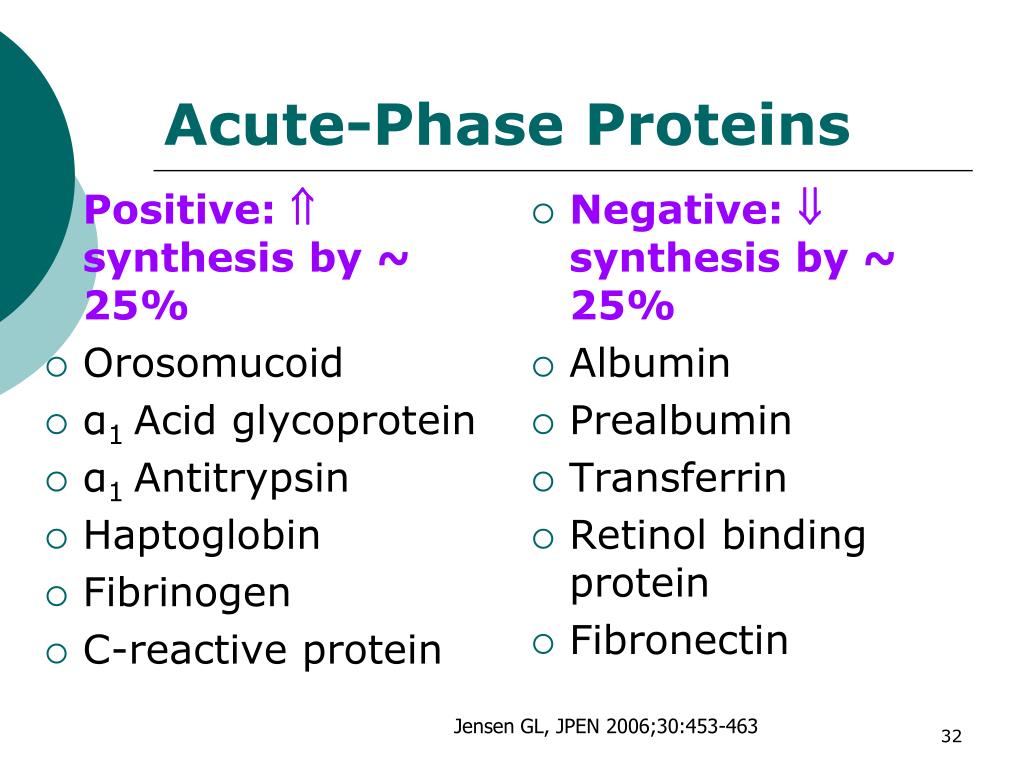
positive acute phase proteins; those that decline are called the negative acute-phase proteins (Tables 4 and 5, respectively). By definition, an acute-phase protein changes by at least 25% during inflammation. Alb, PAB, transferrin, and RBP are expected to return to normal as the inflammatory response resolves. It is clear that these negative.

Acute-phase reactants are proteins whose plasma concentration increases (positive acute-phase proteins) or decreases (negative acute-phase proteins) by at least 25% during inflammatory states. 1 Box 1 lists positive and negative acute-phase reactants. The effect of inflammatory molecules such as interleukin (IL)-6, IL-1, tumor necrosis factor.

The acute phase response. An inflammatory stimulus results in... Download Scientific Diagram
Such proteins are termed either positive or negative acute phase reactants (APR), respectively. The erythrocyte sedimentation rate (ESR), an indirect APR, reflects plasma viscosity and the presence of acute phase proteins, especially fibrinogen, as well as other influences, some of which are as yet unidentified [ 6 ].

What Is The Difference Between Positive And Negative Acute Phase Proteins Relationship Between
Negative acute phase reactants are downregulated, and their concentrations decrease during inflammation. Positive acute phase reactants include procalcitonin, C-reactive protein, ferritin, fibrinogen, hepcidin, and serum amyloid A. Negative acute phase reactants include albumin, prealbumin, transferrin, retinol-binding protein, and antithrombin.

Plasma indices of negative acute phase proteins (albumin, retinol, and... Download Scientific
Or third, albumin is known to be a negative acute phase protein, and as such hypoalbuminemia might represent an increased inflammatory status of the patient, potentially leading to poor outcomes. A thorough review of the literature reveals the fallacy of these arguments and fails to show a direct cause and effect between low albumin levels per.